
- A sad and shocking system that diminishes Australia as a nation.
The media release began as follows:
- The Royal Commission into Aged Care Quality and Safety’s Interim Report has found the aged care system fails to meet the needs of its older, vulnerable, citizens. It does not deliver uniformly safe and quality care, is unkind and uncaring towards older people and, in too many instances, it neglects them.
Commissioners Richard Tracey AM, RFD, QC and Lynelle Briggs’s AO investigation into Australia’s aged care system led them to describe the aged care system as “a shocking tale of neglect”.
“The neglect that we have found in this Royal Commission, to date, is far from the best that can be done. Rather, it is a sad and shocking system that diminishes Australia as a nation.”
Entitled Neglect, the Interim Report of the Royal Commission into Aged Care Quality and Safety, which was tabled in the Australian Parliament today, found that a fundamental overhaul of the design, objectives, regulation and funding of aged care in Australia is required.
Joseph Ibrahim of Monash University has a useful overview in The aged care royal commission’s 3 areas of immediate action are worthy, but won’t fix a broken system. The three areas are:
1. Home care packages
At 30 June, 2019 there were 72,062 people* [see note below] waiting on a home care package. Julie Collins, Shadow Minister for Ageing and Seniors told Radio National that people in their 90’s with a prognosis of six months to live were having to wait two years for a package.
The funding is effectively given to the client to choose a service provider on an open competitive market, which can be not-for-profit, or profit-making. When mental powers are diminishing and family members play a role, this whole process can go more than a little strange.
My wife worked in this area for five years after a career of teaching. It’s not an easy gig. Ibrahim is right when he says there is not a standing army of personal carers or health professionals waiting to step in. My wife says she started with a week’s training, followed by a week with a buddy, then worked while doing a TAFE certificate online. She says there was lots of formal and informal training by the organisation with outside speakers etc along the way.
So I don’t know what the form is in the industry, but the organisation she worked for had a high reputation. There was no long preservice training requirement.
Collins is right in saying that there are some obvious priorities, especially with a $500 million underspend sitting there.
2. Reducing the use of chemical restraint
Completely horrific, but fixing it is easier said than done. Can’t be fixed without more staff and a change in culture.
3. Getting young people out
Ibrahim says:
- The third area is stopping the flow of younger people with a disability entering residential aged care – and speeding up the process of relocating those younger people who are already in residential aged care into community living.
And:
- The logistics of building new housing and developing services in areas of need take careful planning and time.
As Ibrahim says, fixing those three is a long way from fixing the system. The full report is due in November 2020.
ABC Insiders today gave the issue a fair workover.
The Government seemed surprised that the interim report made specific recommendations for action. They had been quite happy to kick the can down the road.
We were all diminished by having the silver-tongued Greg Hunt front the cameras. Richard Colbeck is the actual Minister for Aged Care and Senior Australians. Niki Savva in her book says Hunt was among the least liked and trusted by his colleagues.
This government with its small-government values does not inspire confidence that the short and long-term changes will be made.
Jonathan Green in talking to July Collins (linked above) tried the usual ABC schtick of “both sides of politics are equally to blame”. Collins pointed out that Labor had been in power for only six years of the last 20, and that when they were in charge they enhanced aged care with a Living Longer, Living Better package, a staged process that was to be introduced over four years. She said Scott Morrison took $1.2 billion out of aged care in his first budget, and never put it back.
Labor promised improved aged care last election. The Liberals ran a specific scare campaign as well as telling all the oldies and everyone generally that Bill had his hand in their pocket and was going to take all their money.
Sarah Martin at The Guardian lays out the horror of what the Commission has found:
- More than half of the online submissions to the commission raised issues about substandard care, mostly relating to neglect, dignity, personal care, clinical care and medication management. Concerns were also raised about nutrition, malnourishment, emotional abuse, physical abuse or assault, discrimination and restrictive practices.
That sounds criminal. Then:
- The report also highlights concerns about the country’s “ageist” mindset, saying this culture had led to an indifference to how older people were treated, with the conversation about aged care too often about burden, encumbrance and obligation.
“As a nation, Australia has drifted into an ageist mindset that undervalues older people and limits their possibilities,” the report says.
“Sadly, this failure to properly value and engage with older people as equal partners in our future has extended to our apparent indifference towards aged care services.
“Left out of sight and out of mind, these important services are floundering.”
Moreover:
- Staffing problems are also severe, with difficulties finding people who want to work in a sector marked by heavy workloads, and poor pay and conditions. The report also notes a lack of leadership, patchy education and training and a system that signals working in aged care “is not a valued occupation”. Cases where staff and providers are providing “exemplary care” are happening “despite the aged care system in which they operate, rather than because of it”.
According to the commission, the way the system has been framed as a “market” where old people are treated as customers who can shop around for a service is a fundamental failing.
It says that many older people are not in a position to negotiate prices, services or care standards.
“The notion that most care is ‘consumer-directed’ is just not true. Despite appearances, despite rhetoric, there is little choice with aged care. It is a myth that aged care is an effective consumer-driven market.”
In May this year, before the election, Andrew Donegan and Emil Jeyaratnam wrote an article at The Conversation Nearly 2 out of 3 nursing homes are understaffed. These 10 charts explain why aged care is in crisis.
Here’s their story on staffing:
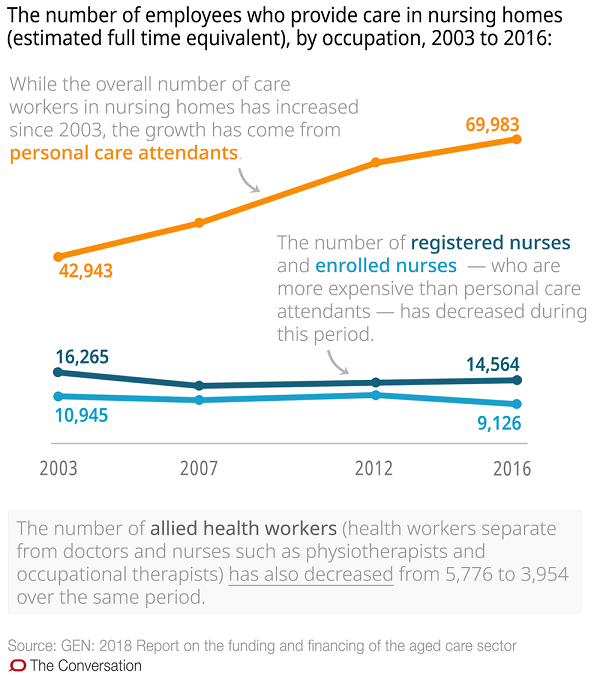
From 2003 to 2016 staff in residential nursing homes ‘personal care attendants’ increased from 42,943 to 69,983, an increase of 63%. At the same time qualified nurses have declined from 27,210 to 23,690 – that’s minus 13%, while the number of allied health workers has declined by 31.5%.
A 2011 Productivity Commission report estimated the workforce will need to grow to about 980,000 by 2050 to meet the demand of aged care consumers, a figure that has since risen. Time we got serious.
We truly need to ask ourselves whether every single person should be treated with dignity, respect, and recognised as having inherent worth. The Liberals and Nationals don’t seem to be able to come to grips with the concept of basic human decency.
* Note:
There is real confusion in quoting figures. Ibrahim cites “72,062 people waiting on a home care package” as at 30 June, but his link takes you an official data report which says this:
- At 30 June 2019, there were 72,062 people waiting on a home care package at their approved level, who had not yet been offered access to a lower level package. Of these people, 95.6 per cent (68,900) had been provided with an approval to access support through the Commonwealth Home Support Program (CHSP).
Commonwealth Home Support Program (CHSP) Guidelines show that the ongoing home care package is but one of four sub-programs. So I think what people are being offered is either high-intensity short-term or episodic help, or alternatively lower-level ongoing support, rather than the real deal.
The shortfall in home care I recall is 120,000, which is what Paul Bongiorno used in The aged care sector is dying for urgent action (whence comes the photo up top) where he also says last year 16,000 elderly Australians died while waiting for their approved home care package.
The whole program costs about $20 billion pa. Increasing funding may just mean more profits for private providers. Biongorno says:
- According to the Tax Justice Network, between them the six largest for-profit companies were given over $2.17 billion in government subsidies – 72 per cent of their total revenue – and made profits of $219 million per year between 2016 and 2018.
One of the 10 charts shows profits peaking in 2016, and then falling in the following two years to land at 2014 dollar levels while presumably expanding. Capital is restless and may go elsewhere for greater rewards.
What the current government is really good at is pretending they are serious when they are not, and then misleading everyone with statistics.
It should also be noted that the Commonwealth Home Support Program (CHSP) Guidelines says the purpose of the program is to meet Australian government objectives. It does not say the purpose is supporting older folk in the community.
Meanwhile Anthony Albanese is campaigning on aged care in Tasmania. That article has a precise figure of “119,524 elderly Australians waiting for a home care packages, including 2115 in Tasmania.” Perhaps sometimes in the outer reaches of the Murdoch empire the truth slips in by accident.

Sorry, Brian
I cross-posted a brief note about expediting Home Care Packages, on a nearby Weekly Salon thread.
Some of we Victorians are somewhat lacking in the telepathy department, and obviously leave a lot to be desired in the foresight area. Didn’t anticipate this here post.
JohnD will blame the high drays. To be more specific, I think it might have been brain damage in younger years caused by falling out of the drays; a tendency to early dementia and loquacity bordering on babble.
Have I had my tablets yet, Nurse?
Rev Ambi: You may not be old enough to remember the pink batt crisis in the distant past when it was claimed that some deaths occurred because the rapid expansion in this activity meant people were starting work on this job without enough training.
The same issues could arise with respect to home care packages. How are extra carers going to be trained and evaluated quickly. How are the systems required to make sure the home care workers are doing a good job. How is the current backlog going to be reduced quickly and the new people who need care are evaluated quickly in future.
Brian may be able comment on the practicalities.
As for falling out of high drays one of my wife’s uncles died after falling off a dray. Take care in your dotage.
We have recently moved to a not for profit retirement village whose services range from independent units for people who don’t need much support to the level of high intensity care that is needed when people are close up or suffering from things like dementia. We moved to this place for a number of reasons:
1. This was the place where my mother lived before she died. We were very impressed with the service she got.
2. It comes with a high care unit that we might need towards the end of our lives. The village is set up so this high care can be provided in our residence if there is no space in the high care section.
3. We moved too far from where we lived to remain part of the community we used to live in and wanted time to establish links with the broader community.
4. In the case of our mothers they went through a burst of rapid deterioration from able to live on their own to needing something that offered more support. The current lag times between sudden deterioration and actually getting the right level of support could be a real problem if one or both of us suddenly has the need for something intensive.
5. We were horrified at the thought of having to deal with a for profit provider where we are no longer able to negotiate effectively.
In terms of negotiating it is important to understand that moving to another village comes at a significant cost. (Part of the problem with Aveo was alleged to be that the company was trying to upset their customers enough that they would leave so that Aveo could pocket the departure fee.
Brian: What is your wife’s view on the desirability of being cared for at home vs being cared for in a specialist village? My take is that the benefits of care at home are being exaggerated.
Ambi, I hate to tell you but I said in the second comment on the other thread that I might do a post on aged care!
I was impressed with what you wrote over there.
No worries. What happens happens.
As I said in the post, my wife had a one week induction course, plus one week with a buddy, then did the TAFE certificate online. So there is no big impediment to getting extra staff.
Mind you, as a casual I think she was paid less than you can make cleaning hereabouts, and she did a lot of cleaning.
Working for older people can be a bit challenging. I have that issue too, but the people I work for don’t suffer from onset dementia. I think most of them prefer me to some young bloke who doesn’t listen.
I recall that in her first week my wife had to call an ambulance because someone slipped on the footpath.
Another was a lady who was hanging up the washing in the back yard with lipstick on and red high-heeled bright red shoes, but nothing on except her underwear. That woman also had a husband who was able.
John, you said:
I’d agree with that, and I think my wife would too.
My younger sister was in an independent living unit, and fought hard to stay there. She made the transition in the middle of this year, and is now happier there than she was alone. I think its 26 residents and there are always two staff there 24/7. The staffing ratio is about right in my opinion, but you will find two staff having to look after multiples of that.
They have organised activities and outings if you want to go.
There is only one registered nurse on the roster, but the others know what they are doing in moving people around, getting the showering and toiletting done etc.
TBH I’ve known others of my generation and a bit older who have been in nursing homes, and haven’t heard a real bad story.
The treatment my sister got in hospital was ordinary or worse, but there was no aggression or mal intent.
In country towns you often have only one choice of a doctor or physio. Sometimes they are a bit below par.
Thanks Brian
I have Early Onset Inattention To Detail.
(Also confess to being Victorian.)
A young lady hereabouts did the TAFE aged care certificate over a few months, not online I think. She will make an excellent carer.
All the staff at the best aged care home I know of, are smiley, careful, engaged with the residents and get on well with each other. It’s a friendly, welcoming atmosphere. Unusual to notice an odour of urine on the premises (First Basic Test of a Facility).
A secure Dementia Ward we saw a decade ago was even cosier and friendlier. Residents enjoyed their time there. Attention to detail by the staff couldn’t be faulted. It included supervised minibus outings.
One of the things that can really make a difference to what happens to a person when they reach the “need care” stage is having a competent, persuasive advocate (like my wife)
on the case. They can work out what sort of places can provide what a person, find a good one and talk the place into accepting the person they are advocating for. They can also keep an eye on what is going on and, if necessary do something to get things fixed.
Too easy to ignore an old person who has no-one to advocate for and keep an eye on them. (Think of the people who, when found have been dead in their house for weeks. We had a tenant who had been dead for a week when the person she had a weekly cup of coffee came around. Could have taken much longer since I suspect the rent was being paid by a routine direct debit.)
Yes John
Luckily some older folk have a family member or dear friend who can advocate effectively.
Also, I hear that newcomers to the NDIS – which is every eligible family – practically require an advocate.*But am also told there are outfits that will act as advocate, for a (relatively low) fee.
* teething problems, lack of experience, differences of interpretation, poorly trained new staff etc.
My wife has now read the post and the comments. She had five years experience, not three, and graduated to being regular part-time, with sick days and super etc.
She says that an important issue in moving to residential care is to avoid a forced move through deterioration of health and/or circumstances.
My sister had this issue. The care she is in is an initiative of local government, the Western Downs. A place became available in Miles, on the same campus as her independent living unit was located. That place became available just when she had had a stint in hospital. The system was willing to support her desire to return to her independent unit through rehab in respite care, but if she chose independence and then had a fall or something a couple of months later she may have ended up in residential care two hours drive away in a town she had never visited in her life.
Brian: Your wife says:
What she says is part of the reason we did what we did. However, avoiding forced moves can be difficult due to time, finance or stubbornness reasons. For example, my mother in law, like many oldies “wanted to stay in her own home” as many do. What finally moved her was a land cruiser backing into and causing enough injury to put her in hospital for a while plus respite time to allow her to recover enough to go back into her home. While there she decided that she rather liked living in a hostel instead of being alone on her own and was lucky enough to have a daughter who could arrange it all. Not sure what would have happened without the daughter.
One of the problems with moving to independent units is that you have to pay for them before moving in and the amount needed usually means having to sell the place the oldie is living in. to make the move my mother had to move into a small rental unit until her house could be sold and she could pay for an interdependent unit. Not always easy to get the retirement village to hold a unit why the house is sold. It is difficult to get a bridging loan if you aren’t working even if you do have plenty of assets.
Having a system that facilitates moves including the supplying of bridging loans would help. Ditto a system with enough spare capacity to allow people to move quickly to a higher level of care when needed would also help. Beats cluttering up hospitals with old people waiting for a place to move to.